Eat Well, Breathe More Easily
Studies suggest that nutrition and dietary changes can improve lung health.

If the eyes are a window to the soul, then the lungs are a door to the body—providing a gateway for the arrival of oxygen to every living cell.
Fitness pros know that regular exercise trains the lungs to inhale more oxygen and exhale more carbon dioxide, improving lung capacity and strength. But can nutrition and eating better make the lungs healthier, too? Though we have much more to learn, the research is promising. Multiple studies provide strong indications that eating certain foods can reverse some lung conditions and may stall the progression of others—or at least improve their symptoms.
Of course, eating right has no adverse side effects. It also benefits other body systems, so focusing on nutrition for lung health is a win-win. Let’s see what research says about the effects of diet on common lung conditions.
Lung Function, Health and Disease

Healthy lungs effortlessly extract oxygen from inhaled air and pass it through tiny air sacs at the end of the lungs’ tubules into capillaries, the smallest blood vessels. From there, red blood cells grab the oxygen molecules and transport them to the heart, which pumps them all over the body. At the same time, every exhalation expels carbon dioxide, the main waste product from cellular activities (NHLBI n.d.a).
Though lungs supply the breath of life, lung health gets a lot less attention than heart disease and cancer, which pose a greater risk of death. Lung diseases include asthma, pulmonary hypertension and chronic obstructive pulmonary disease. According to the Centers for Disease Control and Prevention, nearly 26 million Americans have asthma, while 15 million have COPD (CDC 2013; CDC 2017).
Though lung diseases can be highly treatable, they kill, too. Lung disease ranks fourth in the top 10 causes of death, with nearly 155,000 people in the U.S. dying from some form of chronic lower respiratory disease in 2016 (Xu et al. 2018).
See also: The Science of Breathing
Asthma and What You Eat

Asthma is a chronic condition that narrows the lungs’ airways, inhibiting air flow and causing coughing and shortness of breath (NHLBI n.d.b). Asthma’s exact cause is unknown, but many triggers can cause muscles along the air tubes to tighten and swell. Mucus production may also increase, further narrowing the breathing passages.
People with asthma typically use a mix of medications (such as inhaled corticosteroids) for both long-term control and quick relief from acute symptoms. Some people’s asthma is so severe that they need hospitalization to restore normal breathing.
Tree pollens, air pollution and certain chemical smells can trigger asthmatic responses, as can some animal fur and even exercise. But so can certain foods, such as milk and cheese. For some people with asthma, removing food triggers can work as well as—or better than—taking a medication (NHLBI n.d.b).
“I had an asthmatic patient who was a 27-year-old pharmacy student,” recalls Houston-based Bandana Chawla, MD, who is board certified in internal and lifestyle medicine. “She came in for an appointment and told me that she had gone vegan, had given up dairy, stopped her allergy shots and was no longer using her inhalers.
“I was disappointed and skeptical that this would help her. As I was writing that the patient had been noncompliant with meds in her chart, my assistant was measuring her lung capacity with a spirometry pulmonary function test. To my surprise, her spirometry numbers were improved compared to when she had been managed through medications. I later had a few other patients come in claiming to have cured their asthma by giving up dairy. This led me to review the research, and I ended up going from vegetarian to plant-based, giving up dairy. I also found that I was able to get off the nasal steroids that I had been taking for my own allergies.”
In 2005, an Australian research review didn’t find a definitive connection between dairy and asthma (Wüthrich et al. 2005). But a study in the Journal of Asthma found that subjects with asthma experienced a decline in their pulmonary diffusing capacity for 3 hours after drinking 16 ounces of whole milk (Haas et al. 1991). One research review in the journal Medical Hypotheses found that a milk component called beta-CM-7 could stimulate mucus production in the respiratory tracts of patients with actively inflamed tissues, potentially explaining why eliminating dairy then improved symptoms (Bartley & McGlashan 2010).
Another study experimented with administering a vegan diet—all plant foods and no dairy—to 35 patients who had suffered from asthma an average of 12 years and managed it with medications. Of those who stuck to the eating plan, 71% reported asthma improvement within 4 months. Within 12 months, 92% reported improvement, and there were positive changes in clinical biomarkers such as vital capacity, forced expiratory volume (FEV1, a measure of lung function) and a number of biochemical blood markers (Lindahl et al. 1985).
“I’ve had a number of patients with severe asthma and allergies who, when they switched to eating a plant-based diet, had a resolution of their symptoms,” says Roy Artal, MD, faculty member of the Cedars-Sinai Medical Center Women’s Guild Lung Institute Center of Excellence in Los Angeles and board certified in pulmonology, sleep disorders and internal medicine. “The mechanisms are not entirely understood, but when a patient is looking to avoid being on an inhaled corticosteroid, another option is going on an anti-inflammatory diet, which would be a whole-food, plant-based diet.”
Whole plant foods such as vegetables, fruit, whole grains, legumes, nuts and seeds are high in antioxidants and other phytochemicals that are anti-inflammatory. One study found that ex-smokers who ate more antioxidant-rich apples, bananas and tomatoes over 10 years had a slower decline in their FEV1 than those who ate the smallest quantities of these foods (Garcia-Larsen et al. 2017). The fiber in plant foods may also play a role: One study associated low fiber intake with reduced measures of lung function and an increased prevalence of airway restriction (Hanson et al. 2016). Fiber in plant-based diets feeds the “good” bacteria in the gut microbiome, which then produce anti-inflammatory compounds that can boost immunities and dampen inflammation throughout the body.
See also: Nutrition Hacks Based on Hard Science
CAN SUPPLEMENTS HELP LUNG HEALTH?
One study had people with asthma eat a high-antioxidant diet with seven servings of vegetables and fruit daily, while another group ate no more than three servings. After 2 weeks, those eating the fewest fruits and vegetables had worse outcomes in their lung measures, showing the benefit of greater plant food consumption. Those on the low-antioxidant diet were then given either a placebo or a supplement of lycopene, an antioxidant nutrient in tomatoes and other red foods. After 14 days of daily supplementation, there was no difference in their lung outcomes or measures of inflammation, showing that the lycopene had little effect (Wood et al. 2012).
“I don’t recommend supplements, since it’s generally better to get your nutrients from foods, but you can use some foods as supplements,” says Bandana Chawla, MD, an internist in Houston. “You can add ginger or AMLA powder (which is dried gooseberries) to smoothies or use turmeric and avocado in meals.”
Diet and COPD
Chronic obstructive pulmonary disease is a catch-all term for conditions including emphysema and chronic bronchitis. Smoking is the number-one cause of emphysema, but environmental factors, including diet, may worsen it. Several prospective studies found that adults who ate cured meats (such as bacon, hot dogs and sausage) or processed meats (like ham or deli turkey) on most days of the week had a greater risk of developing COPD. Even after adjusting for smoking, exercise and other potentially confounding variables, regular consumption of these meats posed higher risks than no consumption or consumption less often than once a week (Varraso et al. 2007; Jiang et al. 2008). Researchers theorize that nitrates in cured meats may form reactive nitrogen species that lead to lung damage.
“One study (Keranis et al. 2010) found that people with COPD who followed a plant-based diet high in fruits and vegetables for 3 years experienced a longer preservation in their FEV1 than people who did not,” says Priyumvada Naik, MD, an Atlanta pulmonologist who is board certified in critical care and lifestyle medicine. “I counsel patients to go plant-based to reduce their overall inflammatory burden.”
See also: Plant-Based Power Players
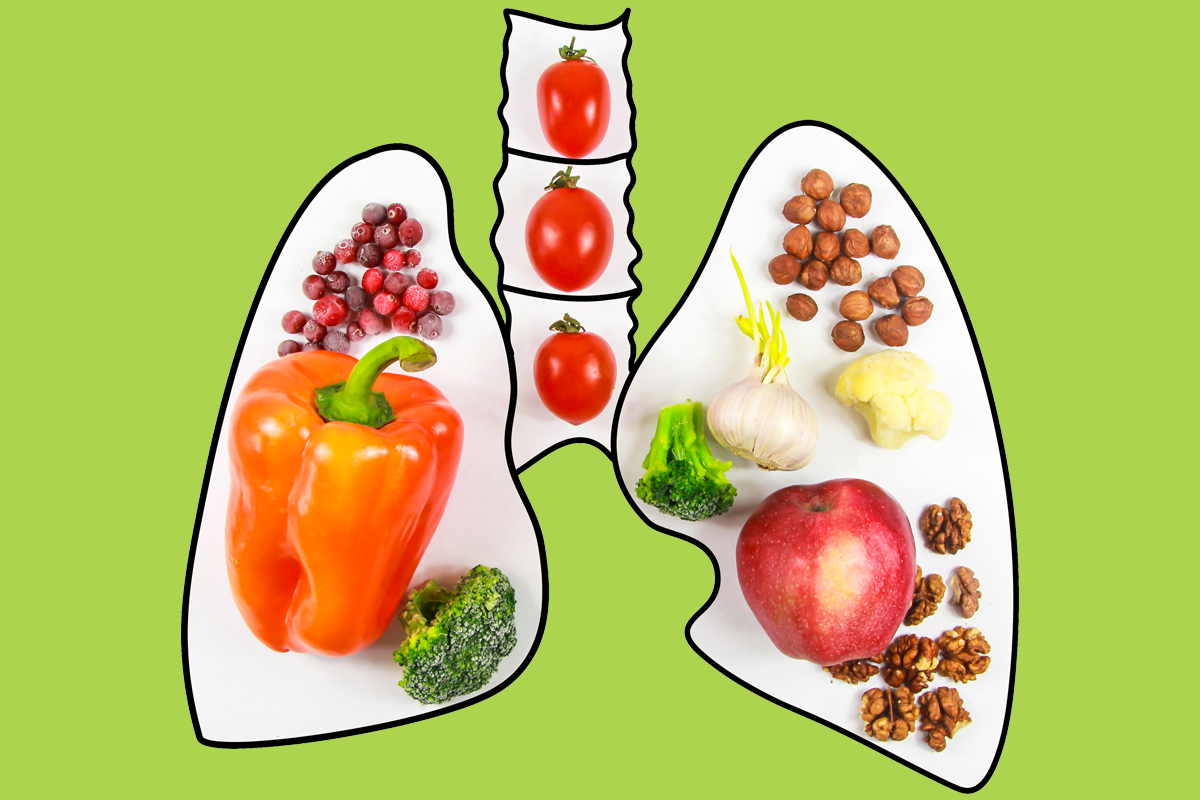
Lung-Loving Foods

While exact diet prescriptions for lung health are unknown, eliminating or minimizing animal foods and increasing consumption of whole plant foods is a good start. Are there any superfoods that might have optimum effects?
One study gave 27 young healthy smokers a daily serving of steamed broccoli (or a control diet) for 10 days. Researchers found that after this regimen, broccoli eaters showed a 41% decrease in free-radical damage to DNA strands in their blood tests (Riso et al. 2010).
“I recommend eating the entire spectrum of plant foods,” Artal says. “Green vegetables should form the core of any plant-based diet, with whole-food starches like potatoes to stay satiated, and nuts, seeds, legumes and whole grains to support protein needs.” He recommends avoiding animal foods because they lack the antioxidant and anti-inflammatory properties of plant foods. “But keep in mind that just being vegan isn’t protection, because you can be an unhealthy vegan eating lots of processed carbs and sugar, which can also be pro-inflammatory,” he says.
Naik agrees that greens can be good for respiratory health: “They induce the production of nitric oxide synthase, which is a vasodilator and, for someone with pulmonary hypertension, can lower PA (pulmonary artery) pressures.”
References
Bartley, J., & McGlashan, S.R. 2010. Does milk increase mucus production? Medical Hypotheses, 74 (4), 732–34.
CDC (Centers for Disease Control and Prevention). 2013. CDC’s national asthma control program. Accessed Mar. 14, 2019: cdc.gov/nceh/information/asthma.htm.
CDC. 2017. Chronic respiratory disease. Accessed Mar. 14, 2019: cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/ChronicRespiratoryDisease.html.
Garcia-Larsen, V., et al. 2017. Dietary antioxidants and 10-year lung function decline in adults from the ECRHS survey. European Respiratory Journal, 50 (6), 1602286.
Haas, F., et al. 1991. Effect of milk ingestion on pulmonary function in healthy and asthmatic subjects. Journal of Asthma, 28 (5), 349–55.
Hanson, C., et al. 2016. The relationship between dietary fiber intake and lung function in the National Health and Nutrition Examination Surveys. Annals of the American Thoracic Society, 13 (5), 643–50.
Jiang, R., et al. 2008. Consumption of cured meats and prospective risk of chronic obstructive pulmonary disease in women. American Journal of Clinical Nutrition, 87 (4), 1002–8.
Keranis, I., et al. 2010. Impact of dietary shift to higher-antioxidant foods in COPD: A randomised trial. European Respiratory Journal, 36 (4), 774–80.
Lindahl, O., et al. 1985. Vegan regimen with reduced medication in the treatment of bronchial asthma. Journal of Asthma, 22 (1), 45–55.
NHLBI (National Heart, Lung, and Blood Institute). n.d.a. How the lungs work. Accessed Mar. 14, 2019: nhlbi.nih.gov/health-topics/how-lungs-work.
NHLBI. n.d.b. Asthma. Accessed Mar. 14, 2019: nhlbi.nih.gov/health-topics/asthma.
Riso, P., et al. 2010. DNA damage and repair activity after broccoli intake in young healthy smokers. Mutagenesis, 25 (6), 595–602.
Varraso, R., et al. 2007. Prospective study of cured meats consumption and risk of chronic obstructive pulmonary disease in men. American Journal of Epidemiology, 166 (12), 1438–45.
Wood, L.G., et al. 2012. Manipulating antioxidant intake in asthma: A randomized controlled trial. American Journal of Clinical Nutrition, 96 (3), 534–43.
Wüthrich, B., et al. 2005. Milk consumption does not lead to mucus production or occurrence of asthma. Journal of the American College of Nutrition, 24 (6 Suppl.), 547S–55S.
Xu, J., et al. 2018. Deaths: Final data for 2016. National Vital Statistics Reports, 67 (5).
Martica Heaner, MA, PhD
Martica Heaner, PhD, MA, MEd, has a weekly column on www.health.msn.com and is the author of several books. She has a doctorate in behavioral nutrition and physical activity and holds two masterÔÇÖs degrees in nutrition and applied exercise physiology from Columbia University in New York City.





