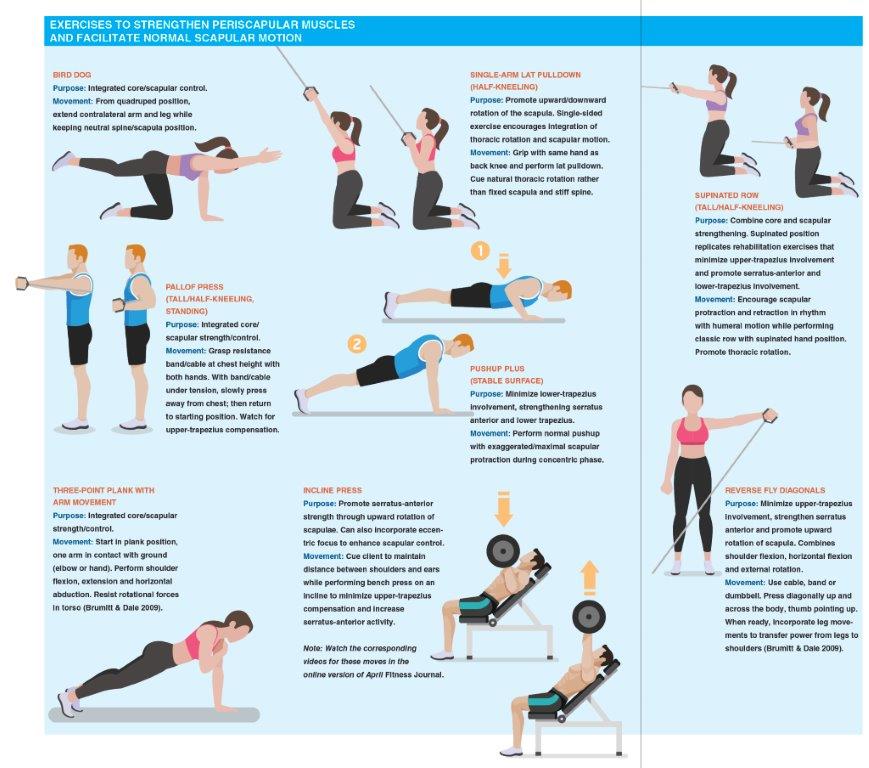
Shoulder Blades: The Right Moves
Here's how to spot scapular dyskinesis in clients and provide corrective exercises.

The shoulder blades, or scapulae, are critical links in the kinetic chain from the waist through the shoulders, up to the neck and down to the fingertips. Abnormalities in the position or movement of the shoulder blades—technically called scapular dyskinesis—can trigger pain and discomfort, especially among people who spend long hours sitting and using computers.
Indeed, more than 60% of us feel neck or shoulder pain at some point in our lives (Cools et al. 2013). A sedentary lifestyle is one of the key culprits because it can impair scapular orientation, range of motion and shoulder muscle strength.
These are crucial issues for fitness pros whose clients complain of shoulder and neck problems. Learning the causes of scapular dyskinesis, spotting the symptoms and finding good exercise options can help restore proper shoulder blade function. This process starts with understanding normal scapular positioning and scapulohumeral rhythm.
Role of the Scapulae
The flat, protruding surfaces of the scapulae provide mobility and stability to the shoulders, neck and upper back, forming a stable base for force transfer from the hips and torso to the arms.
Each scapula has two bony attachments, the acromioclavicular joint and the glenohumeral joint. The absence of bony articulations between the scapulae and the thorax affords great mobility, including retraction, protraction, elevation, depression, anterior/posterior tilting, and internal/external and upward/downward rotation (Kibler, Sciascia & Wilkes 2012; Paine & Voight 2013; Voight, Hoogenboom & Cook 2008).
All this flexibility poses a challenge: Scapular stability and mobility are determined largely by activation of the surrounding muscle. Eccentric control is especially important, because it ensures scapular stability when the arm is moving, is under load or both (Kibler, Sciascia & Wilkes 2012).
Thus, the periscapular muscles are vital to normal shoulder function: They must work in sync to produce efficient movement. The serratus anterior and upper and lower trapezius are the primary contributors and stabilizers of scapular motion (Kibler et al. 2013). Furthermore, the scapulae coordinate with the kinetic chain, transferring forces produced in the hips and torso (Voight, Hoogenboom & Cook 2008), as well as connecting the cervical and thoracic segments of the spine (Cools et al. 2013).
What Is Scapular Dyskinesis?
Scapular dyskinesis is a flaw in scapular position and motion. Here’s how to spot it:
Position. Look for prominence of the medial border and/or inferior angle (winging/anterior tilting of the scapula).
Motion. Look for disrupted rhythm exemplified by early scapular elevation (shrugging of the shoulders) and rapid downward rotation (Kibler et al. 2013).
Though scapular dyskinesis is not an injury, it is associated with many orthopedic pathologies (Cools et al. 2013; Kibler, Sciascia & Wilkes 2012). It’s unclear whether scapular dyskinesis causes injuries or merely reflects the body compensating for pain or dysfunction (Kibler et al. 2013; Kibler, Sciascia & Wilkes 2012). Though many people seem untroubled by scapular dyskinesis, the condition may predispose them to neck and shoulder pain or to injury in other parts of the kinetic chain. Hence, exercise professionals should program suitable exercises that minimize injury risk and encourage healthy scapular motion (Cools et al. 2013).
Note: It is not within a fitness professional’s scope of practice to diagnose an injury or “prescribe” therapy. Always work in concert with an allied medical professional.
Looking for Scapular Dyskinesis
Observing the shoulder blades in motion is a reliable way to identify scapular dyskinesis (Kibler, Sciascia & Wilkes 2012). The following test is reasonably reliable (McClure et al. 2009):
- Have the client hold a 3- to 5-pound weight in each hand and raise and lower both arms slowly in forward flexion to maximum elevation 5 times.
- Repeat the process for shoulder abduction (frontal plane).
- Observe each scapula’s motion, watching for medial-border/inferior-angle
prominence and dysrhythmia, including premature elevation, excessive motion, and/or rapid downward rotation or shrugging of the shoulders (Cools et al. 2007).
Looking Choosing Exercises
Exercises should emphasize proximal stability by strengthening the scapular stabilizers before incorporating complex loaded-arm exercises into a strengthening program (Kibler & McMullen 2003; Kibler & Sciascia 2010). These are the most common motor-pattern alterations in scapular dyskinesis:
- increased activation of the upper trapezius
- delayed activation of the lower trapezius
- weakness in the serratus anterior and lower trapezius
Therefore, select exercises that emphasize lower-trapezius and serratus-anterior activation while diminishing upper-trapezius activation and promoting normal scapular motion (Kibler et al. 2008).
Pushups are suggested for strengthening the serratus anterior and lower trapezius, especially when exaggerated scapular protraction is added at the end of the concentric phase (the “pushup plus”).
A 2014 study found an unfavorable increase in upper-trapezius activity in those with scapular dyskinesis when the pushup was performed on an unstable surface versus a stable surface. The opposite is true for subjects displaying no dyskinesis, suggesting that increased neuromuscular demands from an unstable surface enable the compensatory patterns seen in clients with scapular dyskinesis (Priauá et al. 2014).
It is important to remember that scapular control is part of a larger system. Hip and trunk extension and trunk rotation promote a more retracted and stable scapular position. Therefore, incorporate exercises that promote core and lumbopelvic stability and appropriate spinal mobility. Exercises should promote normal muscle-recruitment patterns that mimic daily or sport-specific activities without compensatory strategies (Cools et al. 2007). The sidebar “Exercises to Strengthen Periscapular Muscles and Facilitate Normal Scapular Motion” identifies suitable exercises to strengthen periscapular muscles and promote healthy scapular motion within the kinetic chain.
Professional Recommendations
Teach clients how to move the scapulae naturally. You can demonstrate proper protraction and retraction during a rowing exercise, for example. Encourage clients to relax their shoulders—rather than shrugging—to minimize upper-trapezius compensatory patterns. It’s also a good idea to perform exercises in a tall/half-kneeling or standing position to increase core muscular activity (Voight et al. 2008), especially for clients who spend most of their days seated.
Incorporating rehabilitation exercises into a warmup routine can prepare the scapular stabilizers for exercise and reinforce healthy motion. If your clients are in pain, refer them to an appropriately trained healthcare provider, such as a physical therapist, for evaluation and treatment.
Better Shoulder Blades
It’s true that scapular dyskinesis does not guarantee injury. Nevertheless, normal scapular function is a vital link in the kinetic chain, so it’s important to select exercises that encourage healthy scapular motion. Start with assessments to determine the presence of dyskinesis. Once you have identified any issues, choose exercises that enhance proximal control of the scapulae and core muscles. Then progress to incorporate functional, multijoint movements with normal muscle-recruitment patterns.
References
Brumitt, J., & Dale, R.B. 2009. Integrating shoulder and core exercises when rehabilitating athletes performing overhead activities. North American Journal of Sports Physical Therapy, 4 (3), 132–38.
Cools, A.M., et al. 2007. Rehabilitation of scapular muscle balance: Which exercises to prescribe? American Journal of Sports Medicine, 35 (10), 1744–51.
Cools, A.M., et al. 2013. Rehabilitation of scapular dyskinesis: From the office worker to the elite overhead athlete. British Journal of Sports Medicine, 48 (8), 692–97.
Kibler, W.B., & McMullen J. 2003. Scapular dyskinesis and its relation to shoulder pain. Journal of the American Academy of Orthopedic Surgeons, 11 (2), 142–51.
Kibler, W.B., & Sciascia, A. 2010. Current concepts: Scapular dyskinesis. British Journal of Sports Medicine, 44 (5), 300-05.
Kibler, W.B., et al. 2008. Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. American Journal of Sports Medicine, 36 (9), 1789–98.
Kibler, W.B., et al. 2013. Clinical implications of scapular dyskinesis in shoulder injury: The 2013 consensus statement from the ÔÇÿscapular summit.’ British Journal of Sports Medicine, 47 (14), 877–85.
Kibler, W.B., Sciascia A., & Wilkes, T. 2012. Scapular dyskinesis and its relation to shoulder injury. Journal of the American Academy of Orthopedic Surgeons, 20 (6), 364-72.
McClure, P., et al. 2009. A clinical method for identifying scapular dyskinesis, part 1: Reliability. Journal of Athletic Training, 44 (2), 160–64.
Paine, R., & Voight, M.L. 2013. The role of the scapula. International Journal of Sports Physical Therapy, 8 (5), 617–29.
Priau├í, A.L., et al. 2014. Electromyographical analysis of the serratus anterior and trapezius muscles during push-ups on stable and unstable bases in subjects with scapulae dyskinesis. Journal of Electromyography and Kinesiology, 24 (5), 675–81.
Voight, M.L., Hoogenboom, B.J., & Cook, G. 2008. The chop and lift reconsidered: Integrating neuromuscular principles into orthopedic and sports rehabilitation. North American Journal of Sports Physical Therapy, 3 (3), 151–59.